Think of the uterine lining as the warm, comfy bed calling an embryo to come and stay a while. When it comes to making those quarters as cozy as can be, lining thickness can play a big role. Here, we break down why lining thickness matters—and what you can do to give it a boost.
How does the uterine lining change during the menstrual cycle?
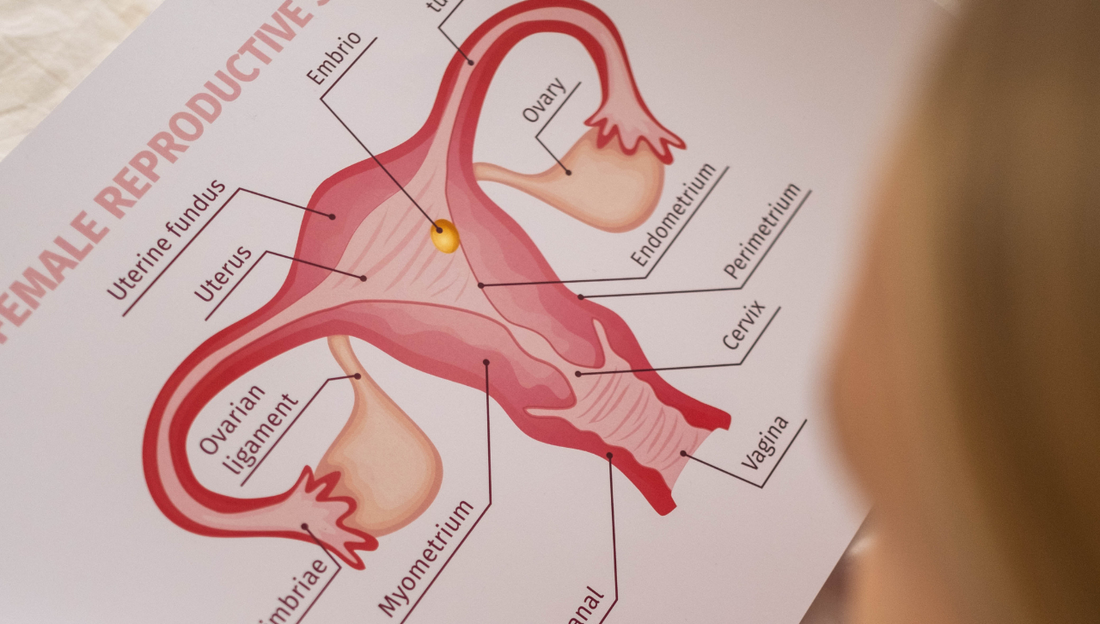
A normal menstrual cycle is made up of two phases. First, the follicular phase is the approximately two-week zone from menstruation to ovulation when a dominant egg, surrounded by follicular cells, starts to grow until its fully developed. In this phase, as the dominant follicle grows, the granulosa cells within it proliferate and they release more and more estrogen. Estrogen is the primary hormone that thickens the endometrium.
The second part—the luteal phase—occurs after ovulation. This is when the dominant follicle releases the egg and becomes the corpus luteum. The main hormone produced by the corpus luteum is progesterone, and it prepares the endometrium to become receptive for an embryo (a fertilized egg) to implant. During this period, the glands of the endometrium change their appearance, becoming dilated and twisty. This leads to changes of the uterine lining as it preps for an embryo implantation.
To simplify, the estrogen in the first phase thickens the lining, and the progesterone in the second phase transforms it into a receptive environment. It is the drop in progesterone that triggers the shedding of the endometrium (a.k.a., menstruation) when implantation doesn’t occur.
Why does uterine lining thickness matter for conception?
Whether you’re trying to conceive on your own or via an IVF embryo transfer, a nice plush lining provides the perfect crash pad for an embryo. Too thin of a lining decreases the likelihood of implantation. In assisted reproductive technologies (ART), most fertility clinics have a threshold of thickness they are hoping to see before proceeding with an embryo transfer, which usually ranges from 6 millimetres to 8 millimetres as the lower limit. Having a lining that’s thicker than eight millimeters has been linked to greater implantation success and higher pregnancy rates.
The way the lining compacts is also linked to conception success. One study found that when the lining reaches eight millimeters or thicker at the end of the estrogen phase and then compacts by 10 percent by the time the embryo is in the uterus, there’s a higher ongoing pregnancy rate (54 percent with compaction versus 21.8 percent without). In ART, a thick endometrium prior to starting progesterone is ideal, and it’s believed that by the time of embryo transfer (usually after five to six days of progesterone) the lining should be thinner (compacted or denser)—which is a good thing! (Compaction is a relatively new concept, so your fertility clinic may not have heard of it or may not be convinced it’s a good marker for implantation success.)
If your lining doesn’t compact, it could indicate an issue with progesterone or your progesterone receptors (the docking ports that progesterone attaches to). For the latter, this is sometimes caused by having an abnormal version of a gene that codes for your progesterone receptors, or it could be related to endometrial inflammation and/or endometriosis.
Is there such a thing as a lining that’s too thick?
If the balance between estrogen and progesterone becomes super skewed, the endometrial lining could start growing abnormally (too thick and with abnormal layers and tissues). This is called endometrial hyperplasia. It’s not uncommon in PCOS patients that don’t ovulate for months (they are just releasing estrogen without progesterone since they don’t ovulate). It can also happen in perimenopausal and menopausal women who are given high-dose estrogen therapy without any supporting progesterone to balance it out for months at a time.
Endometrial thickness is important, but it’s just one variable. Another important one is the pattern of your endometrium that can be seen on ultrasound. Ideally your lining has a trilaminar pattern prior to ovulation (or prior to progesterone start if you’re embarking on an embryo transfer cycle). Speak to your fertility doctor about this variable as well.
What causes a thin lining?
If you’re lining is thin it's important to ensure there is sufficient estrogen levels to stimulate the endometrium to its peak potential. If it remains thin, even with estrogen support, then its important to make sure there isn’t any damage within the uterine cavity. Having scar tissue in the endometrial cavity (A.K.A., Asherman Syndrome) can occur after surgeries or infections and is a common reason for persistent thin lining.
In other cases, poor blood flow through the uterine arteries (the blood vessels that supply the uterus with fresh oxygenated blood) might also interfere with thickening, which is why agents that improve blood flow are often used in an attempt to boost lining thickness and thus, the chance of implantation and pregnancy success, too.
How quickly can the uterine lining thicken?
Generally, your fertility clinic will use estrogen medications (and possibly other medications) for one-and-a-half to three weeks to thicken the lining. If at the end of this time period the lining has not thickened to an ideal state, then you and your doctor will decide how to move forward: with the embryo transfer; trying in the future with another cycle; trying in the future with a different protocol. In medicine very few variables are all or nothing and it’s certainly possible to conceive with a healthy endometrium that’s on the thinner side.
Some linings will struggle more than others to thicken—if you’re in fertility treatment, this is something that is typically closely monitored via ultrasound. Your doctor may prescribe medications to help things along (common add-on medications used to try to thicken the endometrium include aspirin and Viagra), and you can incorporate some healthy lifestyle tips for a well-rounded approach.
How to help thicken the uterine lining?
It's important to discuss a persistent thin lining with your fertility doctor. As mentioned above you need to rule out structural issues like scar tissue. They may attempt some medical approaches like aspirin or Viagra. But there are opportunities for you to optimize your uterine environment on your end. Focus on getting the right nutrients, avoiding environmental and lifestyle toxins, and boosting blood flow to help thicken the uterine lining:
1. Load up on proven nutrients.
Your body needs both Vitamin B12 and Iron to provide healthy, oxygenated blood to your uterus (and your body’s other vital organs and tissues). Vitamin B12 is needed to make red blood cells, while Iron is used to make the hemoglobin in those blood that holds onto fresh oxygen, delivering it around your body. These two nutrients are especially important for vegans and vegetarians since they come largely (or most bio-availably) from animal products.
Vitamin E is well-known as an antioxidant for your cardiovascular system and a protector against blood-vessel damage. It can also affect the genetic expression of cholesterol receptors in the body, acting as an extra defense for blood vessels. All of these actions help with healthy blood flow in the body, including to the uterine lining and new blood vessels that are formed to supply the placenta. One study found that in those who had a previous implantation failure during IVF, taking 400 IU daily of Vitamin E increased lining thickness by 1 millimeter compared to a placebo.
Omega-3 Fatty Acids are often touted for their anti-inflammatory actions, but did you know that they also provide the backbone for making your sex hormones like progesterone and estrogen? Supplementing with Omega-3s (1,190 mg EPA and 795 mg DHA) has also been shown to enhance uterine artery blood flow, as effectively as low-dose aspirin.
(Looking for a prenatal vitamin that packs all these lining boosters? Get Vitamin B12, Iron, Vitamin E, Omega-3 Fatty Acids and more all packed into an easy daily sachet in Bird&Be’s The Essentials for Females or The Power s for Females.)
2. Go organic if you can.
There’s a well-documented connection between chemical pesticides/fertilizers and hormone dysfunction. For example, the pesticide DDT was linked to low luteal progesterone and shorter luteal phases. Foods that contain the highest amount of hormone-disrupting chemicals can be found on the EWG’s “Dirty Dozen” list, which includes strawberries, spinach, kale, apples, grapes and bell peppers. Other foods such as conventionally raised meats, dairy products and processed foods have also been linked to high chemical contamination.
If you can, choose organic produce (prioritize the items listed on the “Dirty Dozen” list if possible) as well as organically fed animal products. Washing and scrubbing your produce with tap water may help remove some pesticide residues, though it’s been found that washing for 20 minutes only reduces residues by about 26 to 63 percent. If you use cleaning solutions like baking soda, soak your produce for at least 12 to 15 minutes to remove 67 to 99 percent of residues.
3. Avoid phthalates.
Phthalates are a group of chemicals and plasticizers that have been linked to reproductive toxicity and infertility, for both ovaries and testicles. They can be found in plastics, synthetic fragrances, perfumes and colognes, personal body products and nail polish.
In the ovaries, high phthalate concentrations can interfere with follicular cells, estrogen levels, and egg development. Plus, phthalates can decrease the ability of endometrial cells to change so that the tissue can thicken to support implantation.
Want to cut back on your phthalate exposure? Replace any personal care products that use “fragrance” or “parfum” unless specifically labeled as “phthalate-free.” You’ll also want to ditch other household products with synthetic fragrances such as air freshers and laundry fabric softeners. When it comes to your food and beverages (whether at-home or take-out), avoid plastics and Styrofoam. Ditch the plastic water bottles and replace them with glass or stainless steel. Swap out any plastic food containers or bags with glass or food-grade silicone.
4. Keep your fiber up—and your carbs low-glycemic.
Maintaining stable blood-sugar levels with fiber-rich foods can help keep arteries dilated for healthy blood flow. Bonus: You’ll be dodging the negative impacts to the bacteria in your gut, vagina and uterus that can be caused by high sugar and low fiber. Although previously thought of as a sterile environment, the uterus actually has its own microbiome: a collection of bacterial species that affect how receptive the endometrium is for embryo implantation. Implantation and pregnancy relies on the uterus having adequate Lactobacillus bacteria. When the endometrium is dominated by healthy Lactobacillus bacteria, implantation rates and live birth rates are significantly higher (60 percent versus 23, and 59 percent versus 7, respectively).
To support your microbiomes, aim for 25 grams of fiber per day and limit or avoid sources of simple sugars such as refined white sugar, white breads, white pasta, white rice, crackers, cookies and pastries.
5. Book in for acupuncture.
Acupuncture has been used for reproductive and gynecological health for thousands of years. By inserting short, thin needles at very specific points in the body, acupuncture can help increase blood flow around the uterus and ovaries, enhancing how the body uses and responds to estrogen, and improving pregnancy rates. In a meta-analysis that looked at 20 different studies, there were significantly greater pregnancy rates in those who did acupuncture, as well as improved endometrial thickness.
6. Make time for exercise.
You probably already know that being sedentary is a major risk factor for cardiovascular diseases. Similarly, sitting all day can restrict blood flow around the pelvic organs and the lower body.
Regular exercise helps protect your blood vessels from stiffening and improves your circulation overall. Plus, exercise is a great way to relieve stress, improve mood, and keep blood sugar and insulin levels managed. This is important since high blood-sugar levels long term can cause blood-vessel damage.
Aim for 30 to 45 minutes of moderate activity most days of the week such as brisk walking, swimming, yoga, low-impact aerobic exercise, dancing or barre.
7. Reach for beets and beetroot juice.
Along with being a good source of Folate, Beetroot increases the amount of nitric oxide (NO) in the body. NO can dilate blood vessels and reduce blood pressure, increasing oxygen delivery to different tissues and organs. How much should you guzzle? Drinking between 140 mL to 500 mL of beetroot juice daily can have positive effects on blood pressure and circulation in as little as three days.
Another perk: Beets also contain Betalains, the special yellow or red/purple pigments in classic beets and in golden beets. These pigments are antioxidants that protect the cardiovascular system. They can improve blood cholesterol, decrease high blood pressure, and decrease homocysteine levels, which is a compound that when elevated has been associated with pregnancy loss and other negative outcomes.
@birdandbe Our co-founder, Breanna, shares what she did leading up to her successful #IVF #embryotransfer. *Disclaimer: Transfer protocols are individualized. Consult your RE before making any changes to your own. #ivfjourney #embryotransfer #ivftiktok ♬ original sound - Bird&Be